What is back pain?
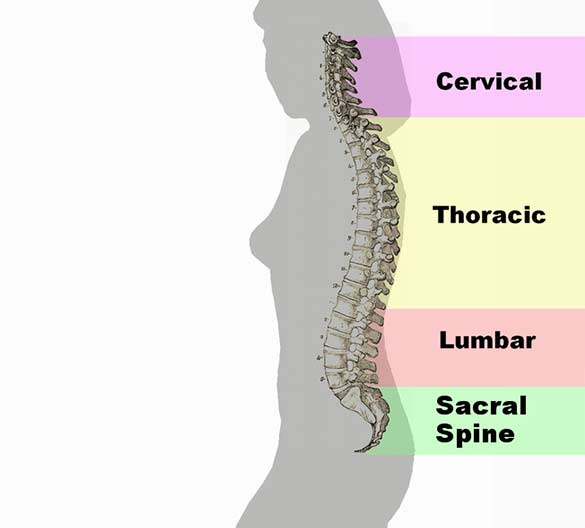
Back pain (also known “dorsalgia”) is pain felt in the back that may originate from the muscles, nerves, bones, joints or other structures in the spine. The pain may have a sudden onset or it can be a chronic pain, it can be felt constantly or intermittently, stay in one place or refer or radiate to other areas. It may be a dull ache, or a sharp or piercing or burning sensation. The pain may be felt in the neck (and might radiate into the arm and hand), in the upper back, or in the low back, (and might radiate into the leg or foot), and may include symptoms other than pain, such as weakness, numbness or tingling. Back pain is one of humanity’s most frequent complaints. In the U.S., acute low back pain (also called lumbago) is the fifth most common reason for all physician visits. About nine out of ten adults experience back pain at some point in their life, and five out of ten working adults have back pain every year. The spine is a complex interconnecting network of nerves, joints, muscles, tendons and ligaments, and all are capable of producing pain. Large nerves that originate in the spine and go to the legs and arms can make pain radiate to the extremities.
- Back Pain Associated conditions
- Back Pain Underlying causes
- Back Pain Treatment
- Back Pain Conservative treatment
- Back Pain Surgery
- Back Pain Emerging Treatments
- Back Pain Treatments with uncertain or doubtful benefit
Back Pain Associated conditions
Back pain can be a sign of a serious medical problem, although this is not most frequently the underlying cause:
Typical warning signs of a potentially life-threatening problem are bowel and/or bladder incontinence or progressive weakness in the legs. Patients with these symptoms should seek immediate medical care.
Severe back pain (such as pain that is bad enough to interrupt sleep) that occurs with other signs of severe illness (e.g. fever, unexplained weight loss) may also indicate a serious underlying medical condition.
Back pain that occurs after a trauma, such as a car accident or fall, should also be promptly evaluated by a medical professional to check for a fracture or other injury.
Back pain in individuals with medical conditions that put them at high risk for a spinal fracture, such as osteoporosis or multiple myeloma, also warrants prompt medical attention.
In general, however, back pain does not usually require immediate medical intervention. The vast majority of episodes of back pain are self-limiting and non-progressive. Most back pain syndromes are due to inflammation, especially in the acute phase, which typically lasts for two weeks to three months.
A few observational studies suggest that two conditions to which back pain is often attributed, lumbar disc herniation and degenerative disc disease may not be more prevalent among those in pain than among the general population and that the mechanisms by which these conditions might cause pain are not known. Other studies suggest that for as many as 85% of cases, no physiological cause can be shown.
A few studies suggest that psychosocial factors such as on-the-job stress and dysfunctional family relationships may correlate more closely with back pain than structural abnormalities revealed in x-rays and other medical imaging scans.
Back Pain Underlying causes
Transient back pain is likely one of the first symptoms of influenza.
Muscle strains (pulled muscles) are commonly identified as the cause of back pain, as are muscle imbalances. Pain from such an injury often remains as long as the muscle imbalances persist. The muscle imbalances cause a mechanical problem with the skeleton, building up pressure at points along the spine, which causes the pain.
Another cause of acute low back pain is a Meniscoid Occlusion. The more mobile regions of the spine, such as the facet joints, have invaginations of their synovial membranes that act as a cushion to help the bones move over each other smoothly. The synovial membrane is well supplied with blood and nerves. When these become pinched or trapped sudden severe pain may result. The pinching causes the membrane to become inflamed, causing greater pressure and ongoing pain. Symptoms include severe low back pain that may be accompanied by muscle spasm, pain with walking, concentration of pain to one side, but no radiculopathy (radiating pain down buttock and leg). Relief should be felt with flexion (bending forward),and exacerbated with extension (bending backward).
When back pain lasts more than three months, or if there is more radicular pain (sciatica) than back pain, a more specific diagnosis can usually be made. There are several common causes of back pain: for adults under age 50, these include spinal disc herniation and degenerative disc disease or isthmic spondylolisthesis; in adults over age 50, common causes also include osteoarthritis (degenerative joint disease) and spinal stenosis,trauma, cancer, infection, fractures, and inflammatory disease. Non-anatomical factors can also contribute to or cause back pain, such as stress, repressed anger, or depression. Even if there is an anatomical cause for the pain, if depression is present it should also be treated concurrently.
New attention has been focused on non-discogenic back pain, where patients have normal or near-normal MRI and CT scans. One of the newer investigations looks into the role of the dorsal ramus in patient’s pain that have normal radiographic evidence. See Posterior Rami Syndrome.
Back Pain Treatment
The management goals when treating back pain are to achieve maximal reduction in pain intensity as rapidly as possible; to restore the individual’s ability to function in everyday activities; to help the patient cope with residual pain; to assess for side-effects of therapy; and to facilitate the patient’s passage through the legal and socioeconomic impediments to recovery. For many, the goal is to keep the pain to a manageable level to progress with rehabilitation, which then can lead to long term pain relief. Also, for some people the goal is to use non-surgical therapies to manage the pain and avoid major surgery, while for others surgery may be the quickest way to feel better.
Not all treatments work for all conditions or for all individuals with the same condition, and many find that they need to try several treatment options to determine what works best for them. The present stage of the condition (acute or chronic) is also a determining factor in the choice of treatment. Only a minority of back pain patients (most estimates are 1% – 10%) require surgery.
Back Pain Conservative treatment
Heat therapy is useful for back spasms or other conditions.
A meta-analysis of studies by the Cochrane Collaboration concluded that heat therapy can reduce symptoms of acute and sub-acute low-back pain.
Some patients find that moist heat works best (e.g. a hot bath or whirlpool) or continuous low-level heat (e.g. a heat wrap that stays warm for 4 to 6 hours).
Cold therapy (e.g. ice or cold pack application) may be effective at relieving back pain in some cases.
Use of medications, such as muscle relaxants, narcotics, non-steroidal anti-inflammatory drugs (NSAIDs/NSAIAs) or paracetamol (acetaminophen).
A meta-analysis of randomized controlled trials by the Cochrane Collaboration found that injection therapy, usually with corticosteroids, does not appear to help regardless of whether the injection is facet joint, epidural or a local injection.
Accordingly, a study of intramuscular corticosteroids found no benefit. Herbal analgesics may also be effective.
Exercises can be an effective approach, particularly when done under supervision of a professional such as a physical therapist. Generally, some form of consistent stretching and exercise is believed to be an essential component of most back treatment programs.
However, one study found that exercise is also effective for chronic back pain, but not for acute pain.
Another study found that back-mobilizing exercises in acute settings are less effective than continuation of ordinary activities as tolerated.
Physical therapy and exercise, including stretching and strengthening (with specific focus on the muscles which support the spine), often learned with the help of a health professional, such as a physical therapist. Physical therapy may be especially effective when part of a ‘work hardening’ program, or ‘back school’.
Massage therapy, especially from an experienced therapist, may help. Acupressure or pressure point massage may be more beneficial than classic (Swedish) massage.
Body Awareness Therapy such as the Feldenkrais Method has been studied in relation to Fibromyalgia and chronic pain and studies have indicated positive effects.
Organized exercise programs using these therapies have been developed.
Manipulation, as provided by an appropriately trained and qualified chiropractor, osteopath, physical therapist, or a physiatrist.
Studies of the effect of manipulation suggest that this approach has a small benefit similar to other therapies and superior to placebo.
Acupuncture has a small benefit for chronic back pain. The Cochrane Collaboration concluded that “for chronic low-back pain, acupuncture is more effective for pain relief and functional improvement than no treatment or sham treatment immediately after treatment and in the short-term only.
Acupuncture is not more effective than other conventional and alternative treatments.”
More recently, a randomized controlled trial found a small benefit after 1 to 2 years.
Education, and attitude adjustment to focus on psychological or emotional causes – respondent-cognitive therapy and progressive relaxation therapy can reduce chronic pain.
Most people will benefit from assessing any ergonomic or postural factors that may contribute to their back pain, such as improper lifting technique, poor posture, or poor support from their mattress or office chair, etc.
Although this recommendation has not been tested, this intervention is a part of many ‘back schools’ which do help.
Back Pain Surgery
Surgery may sometimes be appropriate for patients with:
- Lumbar disc herniation or degenerative disc disease
- Spinal stenosis from lumbar disc herniation, degenerative joint disease, or spondylolisthesis
- Scoliosis
- Compression fracture
- Emerging Treatments
Vertebroplasty involves the percutaneous injection of surgical cement into vertebral bodies that have collapsed due to compression fractures. This new procedure is far less invasive than surgery, but may be complicated by the entry of cement into Batson’s plexus with subsequent spread to the lungs or into the spinal canal. Ideally this procedure can result in rapid pain relief.
The use of specific biologic inhibitors of the inflammatory cytokine tumor necrosis factor-alpha may result in rapid relief of disc-related back pain.
Treatments with uncertain or doubtful benefit
Injections, such as epidural steroid injections and facet joint injections, may be effective when the cause of the pain is accurately localized to particular sites. The benefit of prolotherapy has not been well-documented.
Cold compression therapy is advocated for a strained back or chronic back pain and is postulated to reduce pain and inflammation, especially after strenuous exercise such as golf, gardening, or lifting. However, a meta-analysis of randomized controlled trials by the Cochrane Collaboration concluded “The evidence for the application of cold treatment to low-back pain is even more limited, with only three poor quality studies located. No conclusions can be drawn about the use of cold for low-back pain”
Bed rest is rarely recommended as it can exacerbate symptoms, and when necessary is usually limited to one or two days. Prolonged bed rest or inactivity is actually counterproductive, as the resulting stiffness leads to more pain.
Electrotherapy, such as a Transcutaneous Electrical Nerve Stimulator (TENS) has been proposed. Two randomized controlled trials found conflicting results. This has led the Cochrane Collaboration to conclude that there is inconsistent evidence to support use of TENS. In addition, spinal cord stimulation, where an electrical device is used to interrupt the pain signals being sent to the brain and has been studied for various underlying causes of back pain.
Inversion therapy is useful for temporary back relief due to the traction method or spreading of the back vertebres through (in this case) gravity.
The patient hangs in an upside down position for a period of time from ankles or knees until this separation occurs. The effect can be achieved without a complete vertical hang (90 degree) and noticeable benefits can be observed at angles as low as 10 to 45 degrees.
Back Pain Emerging Treatments
Vertebroplasty involves the percutaneous injection of surgical cement into vertebral bodies that have collapsed due to compression fractures.
This new procedure is far less invasive than surgery, but may be complicated by the entry of cement into Batson’s plexus with subsequent spread to the lungs or into the spinal canal.
Ideally this procedure can result in rapid pain relief. The use of specific biologic inhibitors of the inflammatory cytokine tumor necrosis factor-alpha may result in rapid relief of disc-related back pain.
Back Pain Treatments with uncertain or doubtful benefit
Injections, such as epidural steroid injections and facet joint injections, may be effective when the cause of the pain is accurately localized to particular sites. The benefit of prolotherapy has not been well-documented.
Cold compression therapy is advocated for a strained back or chronic back pain and is postulated to reduce pain and inflammation, especially after strenuous exercise such as golf, gardening, or lifting. However, a meta-analysis of randomized controlled trials by the Cochrane Collaboration concluded “The evidence for the application of cold treatment to low-back pain is even more limited, with only three poor quality studies located. No conclusions can be drawn about the use of cold for low-back pain”
Bed rest is rarely recommended as it can exacerbate symptoms, and when necessary is usually limited to one or two days. Prolonged bed rest or inactivity is actually counterproductive, as the resulting stiffness leads to more pain.
Electrotherapy, such as a Transcutaneous Electrical Nerve Stimulator (TENS) has been proposed. Two randomized controlled trials found conflicting results.
This has led the Cochrane Collaboration to conclude that there is inconsistent evidence to support use of TENS. In addition, spinal cord stimulation, where an electrical device is used to interrupt the pain signals being sent to the brain and has been studied for various underlying causes of back pain.
Inversion therapy is useful for temporary back relief due to the traction method or spreading of the back vertebres through (in this case) gravity. The patient hangs in an upside down position for a period of time from ankles or knees until this separation occurs. The effect can be achieved without a complete vertical hang (90 degree) and noticeable benefits can be observed at angles as low as 10 to 45 degrees.